A Guide to FTM Sexual Health with a Focus on Post-Transition Care
Everyone deserves accurate sexual health care. This goes for Trans men and gender non-conforming individuals. This care may be one of the very things you need if you are transitioning. Sexual health care after transitioning entails any activity, service, or product. These aim to keep your sexual life healthy, safe and in motion.

According to the Human Rights Campaign, trans people have more risk of having HIV. This is compared to the general population. This risk is due to transphobia and marginalization that transgender people face. Still, this does not stop you from taking your sexual health matters into your own hands. You will need STI screenings, HIV prevention, and sexual healing after transitioning. Others include contraceptive health, your post-transition care requires you and your healthcare provider to make a concerted effort. Your body image and self-discovery will thank you for taking care of your sexual health post-transition.

Herein is a guide on FTM sexual health with a keen focus on post-transition care. In this article, you will find answers on how to take charge of your sexual health for a wholesome mind and body.
Understanding FTM Sexual Health
FTM sexual health includes the sexual health needs of FTM individuals and gender non-conforming individuals. Always be ready to take care of your sexual and reproductive health.

It includes gender-affirming products, contraceptive use, and family planning. Others include reproductive health screening. Hormone therapy for transmasculine people also counts.
Some key considerations for sexual well-being during transition include body image and self-discovery.
Body Image

With body image, you get to know which sexual needs matter. Negative body image may affect your sexual health concerns. For example, gender dysphoria causes intimacy issues for many FTM.
Self-Discovery

Discovering the inner bits of your sexual health is the gateway to self-discovery. Many transmasculine people gain confidence and gender euphoria after exploring hormone treatment. This includes surgery for gender alignment.
Hormone Therapy and Its Impact on Sexual Health
Hormone therapy affects you in many ways;
Testosterone Therapy in FTM Transition
Testosterone therapy is a significant part of the FTM transition for trans men. This goes for those who want to develop male secondary characteristics. You receive the hormone testosterone via injection, patch, or oral dose.

Testosterone induces secondary male characteristics in the body. The dose depends on the extent of the secondary male characteristics you need.
Effects of Testosterone on Sexual Function
HRT affects your sexual function and genitals. You may feel more aroused. You may want to masturbate often as a result. You may feel gender euphoria, which in the bedroom translates to body acceptance.
Testosterone effects include the following;
- Vaginal dryness and discomfort
Vaginal dryness and discomfort may manifest as a result of hormone therapy. As the levels of testosterone rise, estrogen decreases. Estrogen is the hormone responsible for lubricating your vagina.

It causes thick, supple, and stretchy lubrication. With more testosterone and less estrogen, you get vaginal dryness and discomfort.
- Changes in genital sensitivity
Testosterone causes genital sensitivity. Some trans men report bottom growth. This occurs when the clitoris, labia, or vulva increase in size due to testosterone. The average trans man will notice a bottom growth of about 1-4 cm.
Genital sensitivity happens when the erectile tissue in your lady part becomes enlarged. It can also become stimulated and aroused, which translates to genital sensitivity.
Practical Tip
Use of lubricants to manage dryness and discomfort. Lubricants will make your lady parts more receptive to touch. It will manage the dryness and discomfort.
Regular STI Testing and HIV Prevention
Reasons for Regular STI Screening
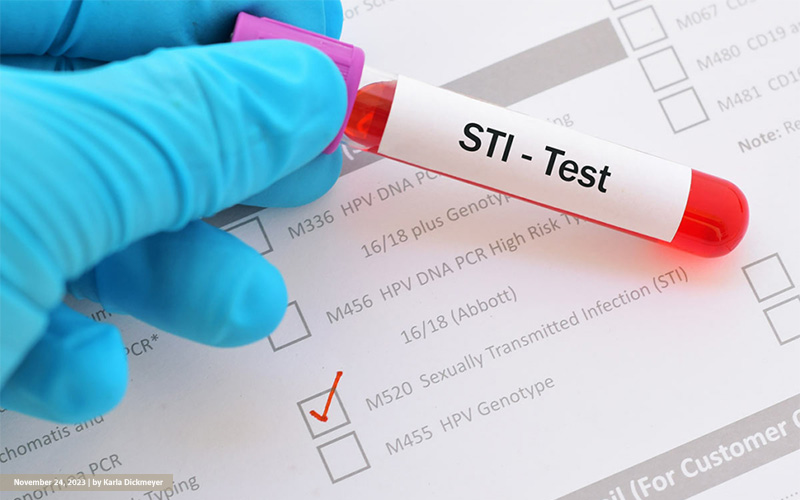
You need to have regular STI screenings as you transition. The goal is to ensure that you are free from STI and reduce your risk of exposure. You can get your STI screenings at your local healthcare.
Key STIs to Check

- There are specific STIs to watch out for to manage your health as a FTM. These include chlamydia which is spread through anal, vaginal, and oral sex.
- Genital herpes caused by the herpes virus. It will affect your skin, cervix, and genitals.
- HIV affects the immune system. It spreads through sexual contact and other means. If you have HIV, you have a higher risk of contracting STIs.
HIV Transmission Risks
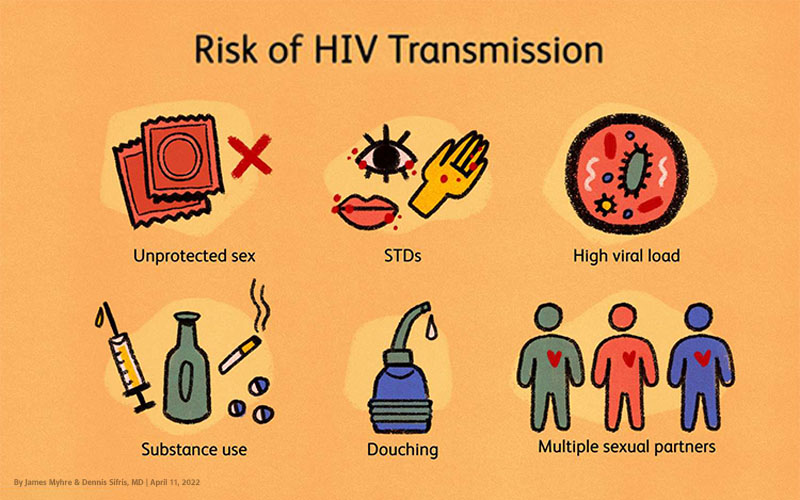
On top of that, knowing HIV transmission risks is important. These include;
- Engaging in anal or vaginal sex without a condom.
- Having another sexually transmitted infection, such as syphilis.
- The use of alcohol or drugs while engaging in risky sexual behavior.
PrEP (Pre-Exposure Prophylaxis)
All exposures that risk you to HIV are not equal. To prevent HIV Transmission, your healthcare provider will give you PrEP. PrEP prevents you from contracting HIV when having sex with a person infected with HIV.

These are given either as an injection or oral medication. The role of PrEP in HIV prevention includes reducing your risk.
A Practical Tip
When it comes to HIV prevention is regular testing. PrEP also aids in HIV prevention as it prevents the AIDS virus from taking hold of your body and spreading.
Post-Transition Care: Sexual Health After Surgery
Post-transition care to heal your sexual life back to health is important.
Impact of Gender-Affirming Surgeries on Sexual Function
Gender-affirming surgeries have positive effects on your sexual function. These gender-affirming surgeries include phalloplasty. This is a surgical procedure. Your healthcare provider will give you a fake penis or implant.

Metoidioplasty is another type of gender-affirming surgery. Here you will have some of your female organs, such as ovaries, removed.
Healing process and sexual activity restrictions
After your gender-affirming surgery, you may need lots of rest. Some surgeries take a day, while others take time. It all depends on how many surgeries you have had, and how long each surgery lasts.

Care include the following;
Care for your wounds, catheters, and drains by washing. Always check for signs of infection such as swelling or bleeding.
Avoid reaching or straining when moving about or reaching out for objects. This is to prevent more injuries.
Monitoring your eating happens for a successful healing. Do this by being in touch with your healthcare provider.
Adjust your routine to include exercise limitations. You also need to avoid sexual activities until you have healed.
Addressing post-surgery discomfort

Do this by;
Taking your medicine as prescribed by your healthcare provider. These include pain relievers and anti-inflammatory medication.
Shared decision-making between you and your healthcare provider is crucial. This will help you manage discomfort after surgery.
Practical Tip
It is always important to follow aftercare instructions. Additionally, lubricants and condoms can help with sore wounds.
Managing Erectile Function After Surgery
Erectile dysfunction where your erection fails can occur after surgery.
Options for Erectile Function Post-Surgery
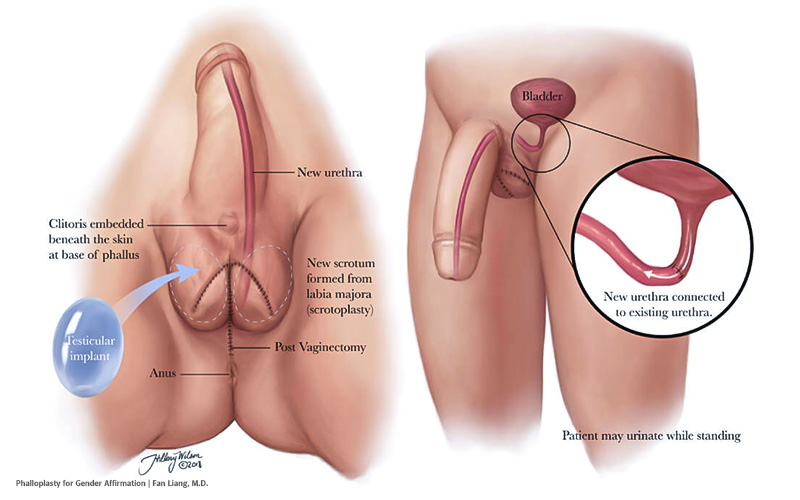
One option for erectile function for trans men is stretching. Post-operative genital stretching after metoidioplasty is advised. This is to reduce genital shrinkage. Other options include
Use of Penile Implants
Inflatable implants are penile implants to help you with erections. They can be filled with air to create an erection. The air can be released. It consists of the following three features;
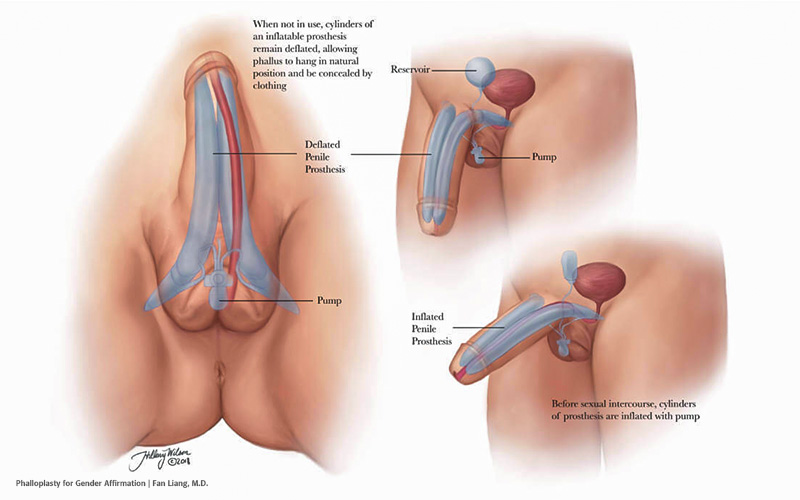
- A fluid-filled reservoir which is placed in your abdominal wall.
- A pump to help create pressure for the implant motion.
- A release valve to help control erection through inflatable cylinders.
Semi-rigid rods are firm devices that will help with your erectile function. They are bent away from your penis for sexual activity. You also pull them toward your body for concealment.
Mental Health and Body Dysphoria in Sexual Relationships
Keeping your mental health in check can help with body dysphoria.
The Psychological Impact of Body Dysphoria on Sexual Intimacy
Body dysphoria can have a devastating impact on your mental health. This can further affect your sexual intimacy with yourself and your partner. It manifests as;

a)Poor body image where you do not feel adequate to engage in sexual intimacy. This may manifest as shyness or refusal to move freely into intimate settings.
b)Low self-esteem, which you will know with feelings of not feeling enough. Body dysphoria may make you feel like the parts that you hate about your body, and your partner does, too.
c)Poor performance occurs. This is when one does not feel fit to engage in certain intimate scenarios. For instance, prior to bottom growth, FTM individuals may feel incompetent.
Navigating Feelings of Discomfort and Anxiety
You have many ways to navigate feelings of discomfort and anxiety in sexual relationships.

a)Gender-affirming products such as packers can help you have sex with your partners. For instance, the pack, play and pee packer for trans men allows you to have sexual penetration.
b)You can enlist the help of therapists. There are specialized therapists in the sexual health of trans men. These can also offer therapeutic solutions.
c)Open communication and transparency with your partner about these feelings is important. Especially feelings of discomfort and anxiety can offer a middle ground to solutions.
Contraception and Pregnancy After Transition
After transition you may want to deal with contraception and pregnancy issues.
The Impact of Testosterone on Fertility
Testosterone may reduce your ability to get pregnant. But it does not stop this ability. As a result, it is wise to always check on your contraceptive options. This will help you manage your reproductive goals.
Contraceptive Options
As a result, it is always important to know your contraceptive options. These are family planning or birth control products that protect you from pregnancy.

- Implants that have a slow-release mechanism. If you are using an implant, it should be about 4 centimeters long. it will release the hormone progesterone in your body.
- Intrauterine devices are small contraceptive devices. These are placed in your womb to prevent pregnancy. In your local stores, you may see them labeled as ‘Mirena’ or ‘Kyleena.’
- Injections as a mode of contraceptive use hormones. For instance, Depo-Provera uses progesterone to prevent pregnancy.
- Vaginal rings are devices placed in your vagina to prevent pregnancy. If you find it hard to remember to take your pill every day, vaginal rings may be an alternative.
- Barrier methods such as the use of condoms and diaphragms are also options. These help prevent sperm from reaching your reproductive tract.
Importance of Using Protective Barriers
Protective barriers such as condoms protect you from STIs and pregnancy. This is why one of the most vouched protective barriers is the use of condoms.
When used correctly, it is an effective barrier against STIs. External condoms such as rubber are worn on an erect penis or a vibrator.

Always discuss your contraceptive methods with your healthcare provider. Discuss your sexual health needs with your provider. You will get the best contraceptive options.
Conclusion
Take pride in yourself. Do this by taking steps to focus on your sexual health after post-transition. You will experience body changes after hormone treatment and surgery. Be ready to nurse your body back to health.

Focus on STI health screenings and preventive barriers. These protect you from sexual health diseases and unwanted pregnancies, respectively. Modern science has made it possible to start up in the bedroom as the man that you are, so by all means, take it.

 Basic Packers
Basic Packers Pack & Play
Pack & Play STP
STP